Requip
"Purchase requip toronto, when administering medications 001mg is equal to".
By: U. Tangach, M.B. B.CH., M.B.B.Ch., Ph.D.
Co-Director, Mercer University School of Medicine
Complications are associated with both methods of treatment; most series show the rate to be higher in patients managed by surgery symptoms 6 days after iui generic 1 mg requip free shipping. The contemporary methods of reducing intraoperative bleeding by preoperative embolization usually are not included in these series rust treatment order requip 2mg free shipping. The intraoperative precision achieved by using contemporary methods surely render previous complication data invalid medicine 1800s purchase line requip. These complications should not occur as long as doses in the 4000- to 4500-cGy range are used medicine keri hilson lyrics discount requip 2mg fast delivery. Fuller and colleagues 171 reported one fibrosarcoma in their series that was considered a radiation-induced malignancy. Malignant transformation of tissue secondary to radiation has been reported in these tumors, and although unusual, this occurrence is a concern. The decision to operate or radiate should be based on a formula that considers tumor size and location, patient age and health, symptoms or signs present before treatment, potential morbidity, and the expertise and availability of those involved in treatment. The decision should be made in consultation between the head and neck surgeon and the radiation oncologist and with an appreciation for the fact that this group of tumors is one of the most complex and dangerous head and neck tumors to be treated. To do nothing is an acceptable option in some patients, because these lesions are often tolerated well and for a prolonged period. In general, a reasonable plan in patients with head and neck paragangliomas is to operate and remove those lesions (whether jugulotympanic, intravagal, laryngeal, or carotid body in origin) that are smaller and less likely to be associated with significant operative morbidity. For large tumors that demonstrate extensive bone destruction, intracranial involvement, or both, or in which considerable operative morbidity is expected, radiation therapy is probably the method of choice for achieving local control. In young patients, radiation therapy should be avoided if a reasonable surgical option is available. On the other hand, the risk for radiation-induced cancer is small, and these authors do not hesitate to recommend it to young patients if the surgical procedure required is likely to be associated with unreasonable morbidity. Older patients are especially suited for radiation therapy, because local control usually is sustained throughout the balance of their lifetime. Removal of jugulotympanic lesions should only be attempted by surgeons trained in otologic and skull base techniques. Those intravagal paragangliomas that are located high in the neck are often very challenging surgical endeavors, being too high to approach by conventional cervical exposure and too low to be handled from an intracranial approach. These are true skull base lesions, often having an epicenter within the jugular foramen. This mostly inaccessible location is best approached by complex but precise and well-described skull base techniques. Fourteen patients were treated primarily, 13 in combination with surgery, and 11 as salvage. Local control was achieved in 79% of the primary radiation group, 100% of the combined therapy group, and 91% in the salvage group. Because resection of vagal paragangliomas is almost always followed by complete vagal paralysis, the choice of a radiation versus a surgical strategy in these lesions should be based on a particularly flexible paradigm. Rehabilitation after resection of midcervical vagal lesions is more easily accomplished than those at the base of the skull. This is partly because of the fact that, in the latter group, multiple cranial nerve injuries are more common. Older individuals have much more physiologic difficulty after vagal nerve resection than do younger patients, regardless of the part of the nerve involved. One must factor into the decision process the fact that a significant percentage of patients with vagal paragangliomas demonstrate a vagal nerve paralysis at the time of diagnosis, and that fact certainly alters the decision process somewhat. Surgery of carotid body paragangliomas, although safe overall, is fraught with hazards, and only head and neck surgeons competent in vascular techniques should attempt to remove these lesions, especially in recurrent lesions. Carotid artery bypass or shunt, or even artery resection and reconstruction, are sometimes necessary to achieve complete tumor removal. Additionally, and with regard to the surgical removal of carotid body paragangliomas, the input from both chemoreceptor and baroreceptor mechanisms is mediated via a common neural pathway; therefore, function of the entire system is affected by the resection of tumors involving the intercarotid paraganglia. Whereas the resection of unilateral carotid body lesions is generally well accepted, excision of bilateral tumors or of a unilateral carotid tumor with a contralateral vagal paraganglioma is often problematic from two standpoints: the potential of sustaining bilateral vagal nerve injury and the baroreceptor dysfunction that potentially can result from the bilateral denervation of the carotid sinuses. Labile hypertension and hypotension, headaches, diaphoresis, and emotional anxiety occur in a substantial percentage of patients who undergo bilateral excision. Considering the gravity of the potential morbidity, we do not recommend bilateral carotid body paraganglioma removal, especially simultaneously.
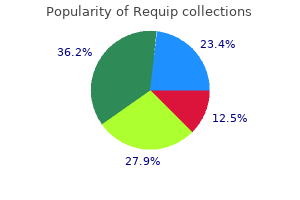
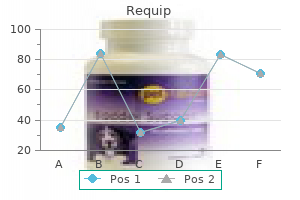
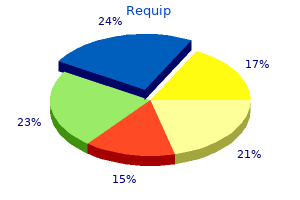
This trial was closed prematurely medicine ball workouts order requip, after 114 eligible patients had been entered medications like zoloft requip 1mg with mastercard, when interim analysis revealed a survival advantage for the radiation treatment arm (P = medications metabolized by cyp2d6 purchase requip with visa. The difference was most marked for patients with clinically positive or multiple histologically positive groin nodes ( medicine xarelto requip 2mg with visa. For patients with two or more positive nodes, the 2-year survival rates were 63% and 37% for the radiotherapy and pelvic node resection groups, respectively. Analysis of failure patterns reveals that the largest difference between treatment groups was in the number of inguinal failures (. With the publication of this study, most practitioners abandoned routine pelvic node dissection, and postoperative radiotherapy became standard for most patients with inguinal node metastases. Survival rates of 114 patients with invasive squamous cell carcinoma of the vulva who were entered on a Gynecologic Oncology Group protocol in which patients with positive groin nodes after radical vulvectomy and bilateral inguinal lymphadenectomies were randomly assigned to receive pelvic lymph node dissection or postoperative irradiation to the pelvis and inguinal nodes (P =. Sites of recurrence in 114 patients with invasive squamous cell carcinoma of the vulva who were entered on a Gynecologic Oncology Group protocol in which patients with positive groin nodes after radical vulvectomy and bilateral inguinal lymphadenectomies were randomly assigned to receive pelvic lymph node dissection or postoperative irradiation to the pelvis and inguinal nodes. Patients who undergo vulvectomy without inguinal node dissection have significantly shorter hospital stays and fewer complications. In a review of 91 patients who had elective treatment of the inguinal nodes for cancers with primary drainage to the inguinal nodes, Henderson and colleagues 678 observed only two recurrences after treatment with 45 to 50 Gy over 5 weeks, and both of these occurred outside the treatment fields. In a retrospective review of 42 patients with invasive vulvar carcinomas, Petereit and colleagues 675 found no difference in the groin recurrence rate for patients with clinically negative inguinal nodes treated with radical lymphadenectomy or radiotherapy, even though the irradiated patients in their series had more advanced primary tumors. The complications of treatment, including lymphedema, wound separation, and infection, and the length of hospitalization were greater for patients who had had lymphadenectomy. Leiserowitz and colleagues 679 reported no groin recurrences in 23 patients with locally advanced, clinically N0 vulvar cancers after prophylactic treatment of the groins with concurrent chemoradiation. The authors concluded that lymphadenectomy was the superior treatment, although the morbidity rate of lymphadenectomy was greater than that of groin irradiation. However, the radiotherapy techniques used in this study have since been criticized. Patients were treated with anterior appositional fields, the dose was prescribed at a depth of 3 cm, and the use of electrons (usually 12 meV) was emphasized. This method of treatment can lead to significant underdosage of the inguinofemoral nodes, which frequently extend to a depth of more than 5 to 8 cm. Some surgeons have tried to reduce surgical complications by reducing the extent of lymph node dissections. Burke and colleagues 641 reported four (5%) groin recurrences in 74 patients with T1 to T2 tumors treated with wide local excision and superficial inguinal lymphadenectomy (unilateral or bilateral depending on the location of the tumor). A number of investigators have explored the use of intraoperative lymphatic mapping to identify a sentinel node that would predict the presence or absence of regional metastases. Further study will be needed to determine whether this procedure can be used to more accurately identify patients who can be successfully treated without the morbidity of radical regional treatment. Treatment of Metastatic Disease A number of reports document the use of single-agent chemotherapy in patients with metastatic or recurrent squamous cell carcinomas of the vulva. In the absence of reliable data specific to carcinoma of the vulva, clinicians often use combinations that have had some activity in the treatment of cervical cancer. However, there are as yet few data to indicate that chemotherapy can provide effective palliation for patients with metastatic or recurrent vulvar carcinoma that is not amenable to locoregional treatments. The continuing increase in adenocarcinoma of the uterine cervix: a birth cohort phenomenon. Oral contraceptives and invasive adenocarcinomas and adenosquamous carcinomas of the uterine cervix. The World Health Organization Collaborative Study of Neoplasia and Steroid Contraceptives. The presence of human papillomavirus-16/-18 E6, p53, and Bcl-2 protein in cervicovaginal smears from patients with invasive cervical cancer. Expression status of p16 protein is associated with human papillomavirus oncogenic potential in cervical and genital lesions. The E6 oncoprotein encoded by human papillomavirus types 16 and 18 promotes the degradation of p 53. Diagnostic cytology towards the 21st century: an international expert Conference and Tutorial. Recent progress in defining the epidemiology of human papillomavirus infection and cervical neoplasia. National Institutes of Health Consensus Development Conference Statement on Cervical Cancer.
Patients with earlier primary-stage melanoma medicine 6 year course order requip 0.25mg mastercard, or patients with metastases to the lungs as the first site of metastasis medicine dictionary order requip american express, had longer postresection survival than other patients treatment 5th disease buy generic requip on-line. The 5-year survival rate for all patients (n = 7564) was 4% treatment jellyfish sting discount requip 1mg online, in contrast to 20% 5-year survival in patients with resection of pulmonary metastases. The lesion may represent a solitary metastasis, a primary bronchogenic carcinoma, or a benign process. The recommended treatment for such a solitary lesion is bronchoscopy thoracic exploration and excisional biopsy. Less desirable is a generous wedge excision and mediastinal lymph node dissection, because local control may be limited. Complete resection of all malignant disease was associated with a 5-year survival rate of 29%. In eight patients with more than one nodule, median survival was 2 years, and no 5-year survivors were reported. In another study of 44 patients, 131 5-year survival after pulmonary resection was 43%. Lefor and colleagues 132 attempted to correlate primary carcinomas of the head and neck with subsequent development of pulmonary metastases or second primary lung carcinomas. The authors recommended that treatment of indeterminate lesions be treated as primary lung carcinomas. Pulmonary metastases from sarcomas or other distinctive nonpulmonary neoplasms are usually easy to diagnose. A generous wedge excision or lobectomy and mediastinal lymph node dissection should be performed. Traditionally, a comparison of the primary neoplasm and the lung nodule using light microscopy has been the only method for determining origin of the lung nodule or neoplasm. Electron microscopy137 or specific molecular or genetic characteristics may identify more precisely the origin of such neoplasms. Monoclonal antibodies can assist in discriminating between primary bronchogenic adenocarcinoma and colon carcinoma metastatic to the lung. Characteristics of metastases and of primary lung carcinoma were examined in an attempt to better direct subsequent therapy. Patients with pulmonary metastases may undergo multiple procedures for re-resection of metastases, with prolonged survival after complete resection. Several studies have reviewed results of multiple resections for recurrent pulmonary metastases. Thirty-four patients were resectable (median survival, 28 months; 5-year survival, approximately 32%). Survival after resection of a solitary recurrent metastasis was 65 months (median) compared to patients with two or more nodules (median, 14 months; P =. At the National Cancer Institute, 70 patients underwent at least one reoperation between 1965 and 1995. The authors noted that complete resection was the most important and favorable prognostic factor. Patients with complete resection had improved survival compared with those who were incompletely resected. Fewer than 3% of all patients undergoing resection of pulmonary metastases will require an extended resection. Pneumonectomy or en bloc resection of pulmonary metastases with chest wall or other thoracic structures, such as diaphragm, pericardium, and superior vena cava, have been performed in a small number of patients with good results. Mortality was 5% and occurred in those patients having pneumonectomy often after multiple prior wedge resections for metastases. The need for pneumonectomy may be evident in the large metastases that involve the majority of one lung and that compress the heart and shift the mediastinum (. In a French study of 42 patients treated over 10 years, 146 29 patients underwent pneumonectomy for sarcoma; 12 for carcinoma; and one for a lipoma. Two postoperative deaths occurred, and four patients had major complications; five patients (12%) had recurrences in the residual lung. The standard surgical mortality for operations for pulmonary metastases is less than 1%. Patients with large centrally located metastases may require pneumonectomy for complete resection. Although mortality for pneumonectomy for pulmonary metastases corresponds to mortality for other histologies, the 5-year survival rate of only 16% demands careful selection of patients before resection.
Pulmonary function after segmentectomy for small peripheral carcinoma of the lung xerostomia medications that cause buy cheap requip 2 mg on line. The influence of surgical resection and intraoperative brachytherapy in the management of superior sulcus tumor treatment 10 purchase genuine requip. Long term clinical and functional results of sleeve lobectomy for primary lung cancer medicine for depression order requip 0.25 mg mastercard. The importance of surgery to nonsmall cell carcinoma of the lung with mediastinal lymph node metastasis treatment croup order requip 0.5mg mastercard. Results of resection in nonoat cell carcinoma of the lung with mediastinal lymph node metastasis. The significance of ipsilateral mediastinal lymph node metastasis (N2 disease) in nonsmall cell carcinoma of the lung. Sites of recurrence in resected stage I nonsmall cell lung cancer: a guide for future studies. Post-surgical stage I bronchogenic carcinoma: morbid implications of recurrent disease. Postoperative radiation therapy in lung cancer: a controlled trial after resection of curative design. A controlled study of postoperative radiotherapy for patients with completely resected nonsmall cell lung carcinoma. Postoperative radiotherapy in nonsmall cell lung cancer: systematic review and meta-analysis of individual patient data from nine randomized controlled trials. The role of post-operative radiotherapy in nonsmall cell lung cancer: a multicenter randomized trial in patients with pathologically staged T12 N12, M0 disease. Bronchogenic carcinoma with chest wall invasion: factors affecting survival following en bloc resection. An appraisal of en bloc resection of peripheral bronchogenic carcinoma involving the Thoracacic wall. The value of adjuvant radiotherapy in pulmonary and chest wall resection for bronchogenic carcinoma. Value of radiotherapy for tumour on the bronchial stump after resection for bronchial carcinoma. Intraoperative 1251 brachytherapy for high-risk stage I nonsmall cell lung carcinoma. The benefit of adjuvant treatment of resected locally advanced nonsmall cell lung cancer. Adjuvant chemotherapy after radical surgery for nonsmall cell lung cancer: a randomized study. Chemotherapy in nonsmall cell lung cancer: a meta analysis using updated data on individual patients from 52 randomized clinical trials. Preoperative x-ray therapy as an adjuvant in the treatment of bronchogenic carcinoma. Preoperative irradiation of cancer of the lung: final report of the therapeutic trial. Chemotherapy followed by lung resection in inoperable nonsmall cell lung carcinomas due to locally far-advanced disease. Surgery and chemotherapy: a new method of treatment for squamous cell bronchial carcinoma. Results of resection in nonoat cell carcinoma of the lung with mediastinal lymph node metastases. Induction chemotherapy prior to surgery for early stage lung cancer-a novel approach. Combined radiation and chemotherapy for unresectable nonsmall cell lung carcinoma. Physical and biological predictors of changes in whole-lung function following thoracic irradiation.
Purchase requip mastercard. Useless ID- Questions+Aswers.